The key things you need to know about root canal treatment
10 November 2022Root canal treatment over time has acquired a lot of negative connotations and association with painful tooth extraction. However, this is very far from the case! Tooth extraction is only a last resort for teeth that are beyond the help of root canal treatment. In fact, by definition ‘root canal treatment’ actually refers to treating the area where the tooth connects to the gums! More commonly known as endodontic therapy, root canal treatment is for removing an infection inside of the teeth and protecting them from future infection. Here’s everything you need to know about root canal treatment.

What is root canal treatment?
To understand what root canal treatment is, we need to understand the composition of a tooth. A tooth consists of ‘the crown’ which is above the gum level, and the roots below which connect it to your jawbone. What connects your tooth to the jawbone are nerves at the pulp (or bottom) of your tooth. This contains nerve tissue, blood vessels and other cells which replenish and strengthen your teeth.
Less costly than tooth removal or dental implants, root canal treatment is essentially the process of removing an infection from the pulp of the teeth. This can occur through cavities from lifestyle behaviours, damaged or cracked teeth, fillings and tooth decay where bacteria can enter the pulp into the roots, and cause infection. If the pulp becomes diseased or injured, it will die which in turn causes the tissue connecting to your teeth to die which causes the pain.
Symptoms of injured or diseased pulp
As a tooth may have more than one pulp, sometimes 3 or 4, there are initial symptoms and symptoms which develop depending on the stage of the infection. Initially you may find:
- You experience pain when eating or drinking hot or cold food or drink
- Pain when eating
- A loose tooth
However an infection may spread, leading to other afflictions such as gum disease. If this is the case you may also experience symptoms such as:
- Pain when eating recurrently
- Swelling of the gum near the affected area
- Swollen cheeks or jaw
- A discolouration in your tooth
If an infection progresses far enough, you may lose symptoms altogether as the infection could have successfully destroyed the root or pulp of your tooth.
So at what point would I need root canal treatment?
Immediately. The longer that the infection has to spread runs the risk of you developing a more serious condition such as Gingivitis (Stage 1 Gum Disease) if not Gum Disease itself. Leaving this may mean that root canal treatment would be unlikely to succeed and it may be easier to extract the infected tooth, replacing it with a dental implant. Removing teeth may affect the appearance of your mouth and cause the other teeth to appear crooked, so root canal treatment can often prevent the need for this. If at any point regardless of if you have these symptoms you experience toothache, you need to contact your dentist.
Common misconceptions
Root canal treatment has built up an unwarranted reputation for being a painful experience. Dentists will never recommend tooth extraction as a first point of call as nothing chews or bites as effectively as a natural tooth. Root canal treatment is actually painless, the pain associated with the treatment comes from the actual infection. Some tenderness is to be expected after the treatment, but a dentist can provide antibiotics on prescription or you can take over the counter pain relief which usually alleviates this.
Steps of root canal treatment
Regardless of whether this is the treatment itself, or tooth extraction, a patient will always be put under anaesthetic unless there are health complications. If proceeding with the treatment then the steps are as follows:
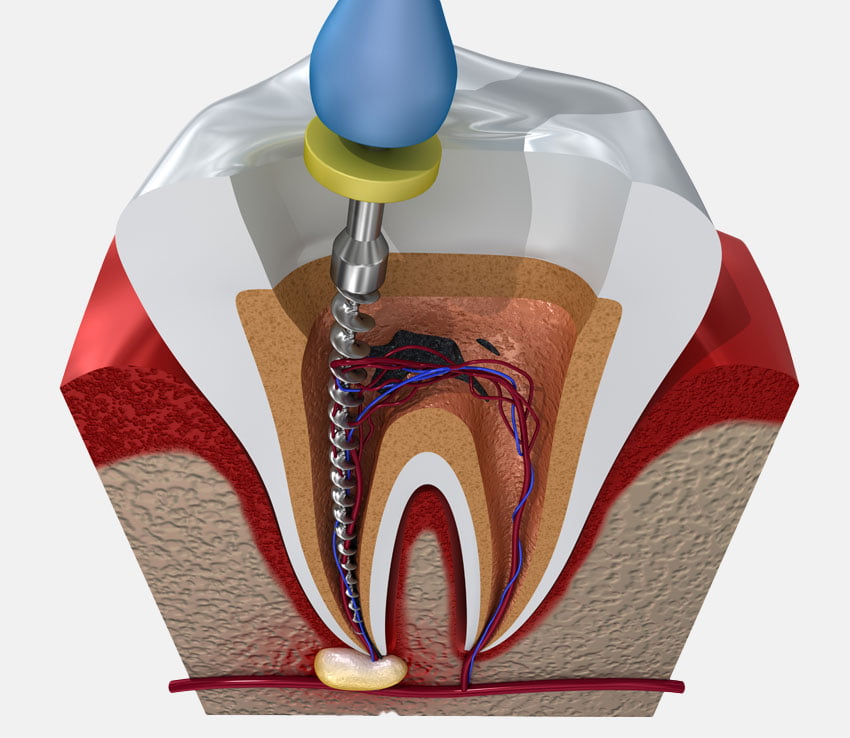
- Cleaning – Firstly, after the anaesthetic has been applied, the dentist will make a small access hole to remove the dead or diseased pulp from the tooth.
- Filling – Using tiny files, the dentist cleans and decontaminates the hollow area in your tooth connecting to the pulp. The tooth is filled with a rubber like material to avoid it becoming brittle and then an adhesive cement is used to seal the canals off permanently to that tooth. Effectively the tooth is dead but can successfully live for up to 9-10 years after!
- Adding a crown or filling – As the tooth may have decayed or deteriorated through the infection, it is now more fragile as it cannot be repaired or replenished by the roots. Adding a crown or filling offers the tooth more protection and helps it to look natural.
All of this can usually be accomplished in one appointment, however, if you have curved or multiple canals, or a large infection then this may need to take place across 1-2 more visits.
Complications
As with any treatment, there are sometimes complications. However, there is not usually much to go wrong. Complications arise if a dentist is unable to find one of the roots, which means the cleaned ones or removed area can become infected again. The infection can also return if the area is not sufficiently filled with adhesive afterwards. The only other area an issue may arise is if the tooth is so infected that it cracks or breaks during the treatment.
Prevention
Of course the best treatment for any dental related matter is by preventing it from happening in the first instance. You can do this by:
- Brushing your teeth twice per day, once before you go to bed and both times with fluoride toothpaste.
- Maintaining a healthy lifestyle in avoiding sugary and alcoholic foods and drinks, stopping smoking, and maintaining a good dental hygiene routine.
- Lastly, by regularly visiting your dentist!
You can book an appointment with ourselves by following the contact information below.
